At the LEDs Magazine Lighting for Health and Wellbeing Conference, speakers covered topics ranging from the perils of shift work and nighttime lighting to the up and down sides of blue spectral energy, as well as the need for better lighting in healthcare facilities, reports MAURY WRIGHT.
This past summer, we held our first one-day immersive Lighting for Health and Wellbeing Conference. The program was exciting, the speakers were passionate, and the field is burgeoning with opportunity. But if there was one phrase uttered more than any other on July 27, it was "It's complicated." Read on for a synopsis of the program and plan to join us at our next event.
Interested in articles & announcements on tunable technology in human-centric lighting applications?
The conference started with a keynote presentation by Shadab Rahman, PhD, who is an instructor in medicine at Harvard Medical School's Division of Sleep Medicine, and an associate neuroscientist at Brigham and Women's Hospital Division of Sleep and Circadian Disorders (Fig. 1). Rahman's presentation focused on circadian issues with shift workers and the potential of circadian adaptation techniques to improve sleep patterns and boost alertness among shift workers.
Shift work is, of course, unavoidable in our society today. Indeed, Rahman pointed out that many first responders — for instance, from fire and police departments — and healthcare workers invariably work on shifts and often face the challenges of working at night and sleeping during the day during a series of workdays, and then transitioning to a normal day/night cycle during a series of off days. Proper rest is a concern for all shift workers, but the examples noted are certainly occupations where alertness is critical.
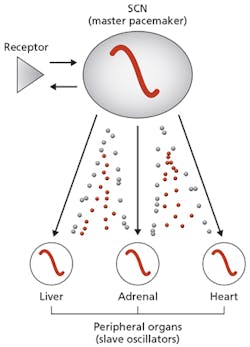
Rahman said, "Shift work forces us to work against our body clock." He described how a master pacemaker called the SCN (suprachiasmatic nucleus) sends out time cues to other physiological systems, and ultimately keeps humans entrained to the 24-hour day (Fig. 2). Essentially, the SCN controls other slave oscillators in the liver, adrenal, and heart areas. Rahman said it's not just sleep but also metabolic and other systems that are impacted by shift work.
There are many factors that can impact these systems, but Rahman described how light has the greatest impact on the 24-hour biological clock. It can be affected by intensity, duration, pattern, history, and wavelength. For example, Rahman said exposure to a lit smartphone is only 30 lx, but its blue-enriched spectrum can delay the clock by an hour and a half, making sleep difficult. He said that a 15-second pulse of light can shift the clock by about an hour. And the impact of light can even be influenced by light patterns a person was exposed to a week or more prior.
Focus on wavelength
Rahman has focused much of his work on wavelength and how it impacts the action spectra of non-visual receptors or intrinsically photosensitive retinal ganglion cells (ipRGCs). We first covered the existence of these receptors in an interview we published back in 2014.
The long-term impact of shift work is not fully understood, although it surely extends beyond sleep issues. Research has suggested it can lead to higher cancer rates, cardiovascular disorders, depression and other mental health issues, gastrointestinal disorders, and more. Of course, lack of sleep caused by circadian misalignment could be in part a factor in the longer list of potential maladies.
So Rahman has done considerable work studying ways to treat circadian misalignment. And we're not talking treatment for symptoms such as sleeping pills to help someone get to sleep, or naps prescribed to increase alertness at other times. Rahman said, "To treat the underlying cause, you have to shift the circadian clock appropriately."
Rahman covered three possible avenues that could help with circadian misalignment among shift workers:
- Complete adaptation
- Partial adaptation
- No adaptation
In a complete adaptation scenario, scientists would look for a way to invert someone's schedule completely. If a work schedule shifts by 12 hours relative to the normal day/night cycle, then the body clock must shift by 12 hours. Partial adaptation might be more easily achieved. In a partial scenario, a work schedule might shift by 12 hours, but perhaps the body clock shifts by only eight or ten hours.
The final possibility — no adaptation — is the most difficult of the concepts to understand. Rahman stressed that it doesn't mean to do nothing. It implies that we pursue techniques, or what neuroscientists call interventions, to prevent the clock from shifting.
The general problem that shift workers face at night is that they aren't typically exposed to a high enough level of light to shift the clock by more than an hour. But Rahman discussed studies of complete adaptation. He said a typical room where workers are present at night might have a 100-lx ambient level and that figure would translate to a biological shift of the aforementioned one hour over the course of a seven-day period of night work.
Rahman said exposing workers to levels between 7000 and 10,000 lx can enable a nine-hour shift over the course of a week. But he added, "Unfortunately, a lot of shift workers don't have seven nights to shift their clock."
International Space Station
Rahman has been involved on a team studying the use of dynamic lighting, entailing tunable correlated color temperature (CCT) or spectral power distribution (SPD) and intensity, that was developed to help astronauts living on the International Space Station (ISS) to adapt to constantly shifting schedules. We first covered the development of the lighting system following a presentation at Strategies in Light back in 2016.
Members of the research team first tested the system aimed at partial adaptation on volunteers in the lab and the system is now being further tested on the ISS. Subjects would be exposed to 6500K-CCT light at a level of 750 lx to instigate a shift. There is a moderate 4500K-CCT mode for normal work. And there is a pre-sleep mode that delivers just 50 lx at 2700K.
The goal of the project was the ability to shift the circadian clock by eight hours. The lab tests realized an actual five-hour shift. The team awaits more results from the ISS, although the system seems like it improves sleep periods and alertness to some extent.
Intervention to adaptation
The final example of research presented by Rahman involved a no-adaptation approach that involved nine nurses tracked for two months, with them alternating between day and night work periods. Basically, the workers wore blue-blocker glasses that filtered the light spectrum under 480 nm. The biggest surprise was that the data indicates lack of blue light exposure didn't increase sleepiness. Rahman said that result was first challenged by other neuroscientists because the prevailing notion has been that blue spectrum increases alertness. Indeed, he said the data caused a number of medical journals to refuse to publish the research, but he also noted that more recent work by other neuroscientists confirms his findings.
Rahman stressed that much more research is needed on the no-adaptation concept, but he clearly believes it could become a viable tool to battle circadian issues. The research on the nurses showed that the intervention did enable the workers to sleep for slightly longer periods during the day while working at night.
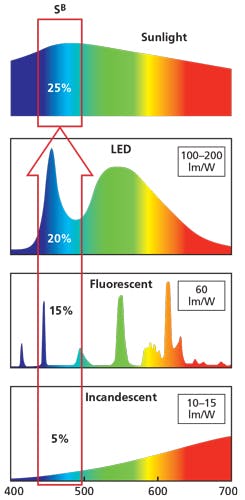
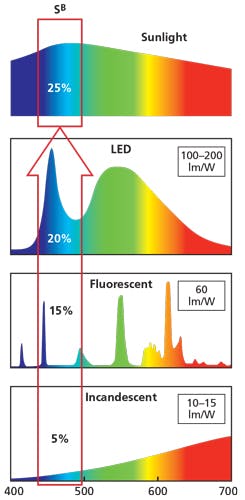
Moving on to other presentations, the discussion of blue-rich light recurred throughout the day of the conference. And the prevailing theme was that blue spectral energy is neither universally good nor bad for humans. It simply depends on when a person is exposed to the blue-rich light that dictates the impact. Moreover, several speakers dismissed completely the notion that the blue emitter or pump used in phosphor-converted white LEDs, is dangerous for the human eye. It was repeatedly pointed out that our eyes get far more blue energy in brief exposure to the Sun than in prolonged exposure to artificial light. A group of researchers in Europe recently reached the same conclusion, as we reported in a news story.
Martin Moore-Ede, M.D., Ph.D., and CEO of Circadian Light, was first to address the issue of blue spectra. Moore-Ede was a professor at Harvard Medical School and led the team that discovered the SCN back in 1980. But it wasn't until 2001 that researchers discovered it was exposure to what Moore-Ede calls "bio-active blue light" as the key to entrainment of the circadian clock. The prior thinking had been that exposure to white light in general was the key.
As Fig. 3 depicts and Moore-Ede detailed, the driver for more efficient lighting has increased the amount of blue energy that we are exposed to indoors — first with the move to fluorescent lamps and later to LEDs. And Moore-Ede described a metric, the Circadian Bio-Active Blue Dose, as the percentage of blue energy in the total spectrum to which we are exposed (SB) multiplied by the intensity (I or total visible irradiance).
Serious health risks
High doses of blue light are acceptable and even preferred during the normal workday as a way to boost alertness and productivity. But Moore-Ede dug into the details of why blue energy has negative impacts beyond lost sleep at night. He cited several organizations, such as the World Health Organization and the American Medical Association, that have published reports associating shift work and circadian disruption to serious health issues. But he said we now understand the causal chain of what is happening.
For instance, consider the increased rate of breast, colon, and prostate cancer associated with people working at night. Moore-Ede directly attributed that hazard to blue light disrupting the circadian clock, thereby suppressing melatonin release by the pineal gland. We have written many times that melatonin is thought to be needed to induce restful sleep, but it is important for other reasons. Moore-Ede said cancer tumors grow 2–3 times faster when melatonin is suppressed. He suggested that the body would fight and even heal small tumors with proper melatonin levels, but the tumors grow to become problematic without the hormone present at the proper levels.
There is also a causal chain that Moore-Ede discussed relative to the claimed increase in obesity and diabetes among shift workers. He said after as little as two nights of exposure to blue light at night, the body develops an increased insulin resistance. Moreover, he said circadian disruption also disrupts the insulin release from pancreatic beta cells.
Circadian Light is, of course, an entrepreneurial company and is selling LED lighting on a commercial basis that would presumably eliminate the blue light issue. The fixtures use a violet emitter and have a depleted, almost non-existent amount of energy in the bio-active blue range.
The company, however, has completed some impressive research in its own small sleep center where volunteers have lived and worked 24 hours a day in what the company called a light-controlled facility. The company has run studies on volunteers making two visits, one with conventional white LED lights and another with Circadian blue-depleted luminaires. Moore-Ede showed data suggesting that the blue-depleted lights eliminate melatonin suppression and also reverse appetite increases that the test documented under the standard white LED fixtures.
Non-image-forming effects
Jamie Zeitzer, PhD at Stanford University, presented a talk entitled "Biological impacts of human centric lighting," and speaking late in the program said he would try and draw a thread through many of the different topics discussed during the day (Fig. 4).
He started by introducing the term NIF (non-image-forming) effects. And it seems there is a subtle difference between that phrase and the more common discussion of non-visual effects. Zeitzer said, "There are a tremendous amount of things that light does in the human brain besides just forming images." As an example, he said if you were exposed to 20,000 lx indoors you would perceive it as very bright uncomfortable light; however, if you walk outside on a nice day into 20,000 lx your perception is that it's quite nice, so there is also apparently a gain-setting mechanism in the mix.
Zeitzer showed data that suggested the NIF response to changing light levels is dependent on background or the light to which a person has been recently exposed. For example, if you are exposed to very low light levels, such as in a lab setting, and then to a brighter light pulse, his research would show that circadian disruption and melatonin suppression are the greatest at just over 100 lx. Moreover, he said if you are exposed to a lot of light during the day, your body may not respond as adversely to light exposure at night. Zeitzer noted, "The research all shows that we have the capacity to respond to this type of light, not that we will respond to the light."
Blue sensitivity is not an exact science
Zeitzer was moving into a discussion of smartphones and tablets and the impact of blue light exposure. He said he would worry more about what someone is doing on such a device at night as opposed to the blue light. If it is a relaxing experience, the positive impact would outweigh the potential impact of the blue light in terms of a circadian disruption, according to Zeitzer.
Zeitzer further warned about focusing just on blue light and on not understanding fully the interactions between cones and melanopsin at different times in terms of chronological exposure to light. He said, "We are not at the point where we understand enough to make actual recommendations in terms of exactly the patterns of light that are necessary to change a person's health or behavior."
The last warning from Zeitzer came relative to human behavior. He asked the question, "Does changing biology change behavior?" He then related a study focused on a group of teenagers. People have suggested that shifting the circadian clock in teens could provide them more sleep. He said, "We changed their biology and all we really came up with was a very complicated way to piss teens off." The message was that changing light does not change behavior, and behavior is different in each situation. In a hospital, for instance, nurse behavior could impact a planned lighting scheme for a patient because the nurse needs extra light to read or perform an examination in a patient room.
Preventing health issues
But not all presentations on the day were on non-visual impacts of light. Deborah Burnett, principal of the Benya Burnett Consultancy, focused her talk on how quality light can impact human health by making sure that practitioners in healthcare can properly assess patients (Fig. 5).
Burnett said the first thing that doctors learn in medical school is the protocol for assessing a patient. And the eye is ultimately the most important tool doctors have, especially to detect skin conditions that are "tells" for doctors, even for serious conditions such as sepsis or cyanosis. Burnett presented several disturbing cases where under poor lighting doctors had missed "tells" that would have indicated a looming drastic situation.
Ultimately, Burnett was championing an algorithm for characterizing the SPD of general lighting products used in healthcare facilities, which would enable doctors the best shot at an accurate assessment. The technology emerged many years ago from the lab of Stephen Dain, professor at the University of New South Wales in Sydney, Australia. The algorithm measures the cyanosis observation index (COI) of a luminaire and is an indication of sufficient energy in the 660-nm red area of the SPD and the presence of cyan. These energy bands are often not in general lighting products because adding red energy adds to cost and hurts energy efficiency. Burnett said researchers found "this was the most critical factor for the human eye to be able to correctly assess the reflectance of blood and other areas that are important for blood evaluation."
Cyanosis observation index
Today, there are few luminaires on the market in most of the world that garner a passing score on the COI metric. Exceptions are in Australia, Japan, Sweden, and a few other countries where compliance is required for luminaires to be used in healthcare settings.
Ultimately, Burnett's message was targeted at lighting manufacturers that need to add products with the required red spectrum. She said the US faces a crisis with more hospitals closing each year and more care being outsourced to places such as retail clinics or what she called a "doc in a box." All would ideally get lighting that complies with the COI algorithm.
The proof is in numbers. For instance, in the area of sepsis, the US has around 500,000 deaths annually related to sepsis and the mortality rate in the US is 40–60%, according to Burnett. She said Australia has a mortality rate of 15% and suggested the difference is the COI lighting that leads to earlier detection because doctors can accurately assess skin.
As you can see, our first Lighting for Health and Wellbeing Conference was information packed and the field is in its infancy. It will be a significant profit opportunity for lighting manufacturers. But it will take diligence. We hope to help. We will soon be planning our conference for next summer and we will have a similar European event. Watch our website for details (lightingforhealthandwellbeing.com). Meanwhile, we will have a few lighting for health talks at Strategies in Light (strategiesinlight.com) in February.
Learn more
SSL impacts speak and the lighting industry listens
As you can see, we've invested a lot of time into delivering the latest thinking on lighting for health and wellbeing, via the conference as well as the pages of our magazine issues and on our website. In our coverage, you will find an interesting transition from human-centrci lighting research to designed studies to installations that are showing the potential of well-designed and implemented SSL to influence the human experience and condition. Look forward to more lighting for health and wellbeing in our next issue.