The current pandemic has focused the public’s attention on infectious disease and its transmission. While disease transmission has always been an important consideration in acute healthcare, it has become increasingly critical in non-healthcare applications, including educational, commercial, indoor recreational, and retail spaces. While the most effective mitigation is vaccination, other precautions such as physical barriers (masking), distance (social distancing), and limiting exposure time have proven to be helpful. The role of the environment in disease transmission through contaminated surfaces or contaminated air is well established, beginning with the father of modern surgery, Joseph Lister, who said, “It is not the air, it is something in the air.” Subsequent observations that sunlight heals wounded soldiers by Florence Nightingale in 1863 and that sunlight kills tuberculosis (TB) by Robert Koch in 1890 formed the basis for the commonly understood principles of ultraviolet (UV) disinfection today.
For a time, many hospitals used UV lighting in occupied spaces, such as operating rooms and patient rooms, to reduce the risk of infection for patients with portals, such as surgical wounds and catheters, for disease-causing organisms to enter. This also acknowledged the role that occupants — the healthcare providers and even the patient themselves — play in disease transmission.
However, the potential safety hazard posed by UV lighting in those applications was not well understood or accounted for. Reports of skin erythema and photokeratitis from surgical staff led to the use of personal protective equipment (PPE) that was cumbersome and interfered with their ability to work. Today, the use of UV light in occupied operating rooms is nonexistent as many hospitals have turned to safer interventions designed to reduce surgical site infections (SSIs).
Upper-air UV, where UV radiation is emitted in the room but largely confined to a portion of the room volume near the ceiling, has been used in occupied patient rooms, specifically those for TB1. Unfortunately, numerous reports have detailed exposure to room occupants due to improper product installation or room design, and to maintenance staff servicing lights or other equipment near the ceiling.
A whole-room approach
Advances in technology coupled with changes in healthcare reimbursement policy created a financial opportunity for whole-room disinfection technologies to reduce healthcare-acquired infections (HAIs). However, the use of UV light was generally limited to unoccupied rooms or enclosed spaces, such as air ventilation systems2. Approaches using visible light and hydrogen peroxide have subsequently been introduced3,4.
Regardless of the mode of disinfection, all systems are engineered and optimized for a particular application and carry with them advantages and disadvantages. The most obvious constraint is room occupancy during disinfectant application.
Due to the nature of how infectious disease spreads, people remain a primary source of pathogens through skin flora and respiratory activity. Therefore, disinfectant application during room occupancy is desirable, but, with the exception of visible light and more recent use of dry-hydrogen peroxide systems, this same disinfectant is typically toxic to humans and only used in unoccupied rooms. As a result, a whole-room disinfection system is not a magic bullet that can replace best practices related to environmental hygiene, sterile processing, and personal mitigation, such as vaccination, masking, and social distancing.
The remainder of this article, the first in a two-part series, will focus on the critical factors, namely safety and industry standards, that potential users should consider when selecting a whole-room disinfection system. The second article will focus on source lifetime, environmental and operational impact, and efficacy.
Safety
The safety of occupants is the most important consideration for a whole-room disinfection system. It drives all other decisions with some options limiting use to unoccupied periods only. No government agency currently oversees the safety of systems that use UV or visible light as the disinfectant. The Food and Drug Administration regulates the use of medical devices whose primary intent is to treat people; the Environmental Protection Agency regulates the use of chemical disinfectants; and the Occupational Safety and Health Administration regulates ionizing and/or coherent radiation. Fortunately, a well-established standard by the International Electrotechnical Commission5, IEC 62471, covers the safety of UV and visible light based on human- and animal-injury data.
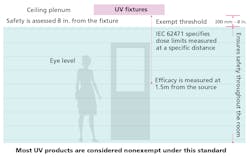
This standard assesses the photobiological risk to human health based on the wavelength of light and its irradiance (or luminance for visible light) at a fixed distance of 200 mm, as shown in Fig. 1. This distance is critical to the assessment and, when applied to whole-room disinfection, ensures safety throughout the room. A product tested against IEC 62471 can receive one of four designations — Exempt or Risk Group 1, 2, or 3. The Exempt designation means no discernable risk exists over an eight-hour period; humans can be exposed to it without the need for exposure controls. Conversely, Risk Groups 1, 2, and 3 require some type of hazard mitigation, depending on the hazard type (UV-C, UV-A, or Visible); these designations also require exposure control, typically through interlocks designed to deactivate the system when the room is occupied. This makes the technology noncontinuous, or episodic, reducing its overall efficacy.
Users can seek this voluntary but effective standard for guidance. It is not intended to cover the use of disinfecting light in contained products, such as air handlers, where exposure to humans is unlikely. It also does not apply to upper-air disinfection units, which can attempt to mitigate the hazard by directing the light away from occupants toward the upper portion of the room (typically 2 ft from the ceiling down). Of course, this does not help people who need to access this upper space (typically for maintenance) or in situations where the wrong product is specified, shipped, or improperly installed.
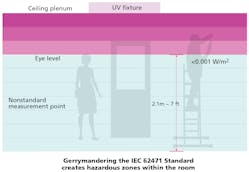
The pandemic has created tremendous interest for products that can mitigate the SARS-CoV-2 virus, including germicidal light. In spite of the inherent resistance to and dangers of this technology, many lighting manufacturers, seeing an opportunity, jumped in with a range of UV products, which would be classified as hazardous under IEC 62471. To overcome these objections, some manufacturers are leading an effort to rewrite existing safety standards or to create new ones by changing the way in which the photobiological assessment is performed. However, testing UV light in a lab is not the same as testing in real-world settings with myriad variables. UV light is a hazard no matter how one does the math or measurements.
Standard testing specifics
IEC 62471, the current standard for photobiological safety assessment, specifies a dose at which the assessment is performed, as well as a distance — 200 mm (approximately 8 in.) from the source.
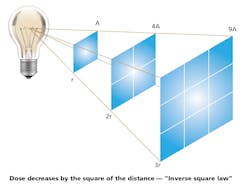
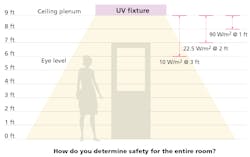
The recently proposed standards suggest measurement 7 ft from the floor. In a room with 9-ft ceilings, this is equivalent to moving the assessment to 24 in. from the source rather than approximately 8 in. As the irradiance at that point (or source luminance for visible light) decreases by the square of the distance (1/R2), this has the effect of reducing the exposure to humans at that point by approximately 1/9. This is shown in Fig. 2.
While the math may be confusing, a simple illustration can highlight the unintended consequences of this effort. Figure 3 shows how the proposed standards could create potentially hazardous zones in the room. While these zones are typically unoccupied, maintenance personnel may need access; in an educational setting or mental-health institution, someone could climb on a desk, chair, or bed and potentially expose themselves to UV radiation.
The responsible approach to UV products is to fully characterize the hazard as existing throughout the entire room and communicate it to users, who should then inform occupants of potential risk.
The simplest way to avoid this issue is to demand a test certificate against the entire, scientifically objective IEC 62471 standard, rather than the commercially driven standards being proposed. In doing so, users can decide what risk they are willing to accept and communicate that to occupants. This eliminates the potential confusion and responsibility shifting among the contractor, building owner, specifier, testing laboratory, and product manufacturer.
Summary
While a plethora of germicidal lighting is coming to the market, not all of it is safe for humans or optimally effective against airborne pathogens. As with any technology, education is key. Fully understanding the advantages and disadvantages of UV light — particularly because it is associated with potential hazards — can help avoid problems.
This is the first article in a two-part series examining disinfection and 405-nm technology. The next article will address source lifetime, environmental/operational impact, and efficacy.
REFERENCES
1. Department of Health and Human Services, “Environmental Control for Tuberculosis: Basic Upper-Room Ultraviolet Germicidal Irradiation Guidelines for Healthcare Settings” (March 2009).
2. T. Ethington, S. Newsome, J. Waugh, and L.D. Lee, “Cleaning the air with ultraviolet germicidal irradiation lessened contact infections in a long-term acute care hospital,” Am J Infect Control, 46, 482–486 (2018).
3. M. Maclean et al., “Environmental decontamination of a hospital isolation room using high-intensity narrow-spectrum light,” J Hosp Infect, 76, 247–251 (2010).
4. J. Sanguinet and C. Edmiston, “Evaluation of dry hydrogen peroxide in reducing microbial burden in a healthcare facility,” Am J Infect Control, 49, 985–990 (2021).
5. IEC 62471, “Photobiological safety of lamps and lamp systems,” CEI/IEC 62471:2006.
Get to know our expert
CLIFFORD J. YAHNKE, PhD, chief scientist and head of clinical affairs for Indigo-Clean and Kenall Manufacturing, may be reached at [email protected]. Indigo-Clean is a registered trademark of Kenall Manufacturing Co., a Legrand company. Kenall was founded in Chicago in 1963 and has built a reputation for durable lighting solutions. Today, the company creates solutions for the healthcare, cleanroom/containment, food processing, transportation, high abuse, and correctional lighting markets. Kenall luminaires are designed in Kenosha, Wisconsin, and comply with the Buy American Act (manufactured in the United States with more than 50% of the component cost of US origin). For additional information, visit indigo-clean.com.
Kenall offers lighting solutions that include 405-nm disinfection technology.
Additional reading
UV-C: Near or Far - Q&A with Bob Karlicek of LESA
Confusion about disinfection light can be dangerous for people and detrimental to the SSL industry
Medical facilities need GUV for pathogens unrelated to the COVID-19 pandemic
For up-to-the-minute LED and SSL updates, why not follow us on Twitter? You’ll find curated content and commentary, as well as information on industry events, webcasts, and surveys on our LinkedIn Company Page and Facebook page.